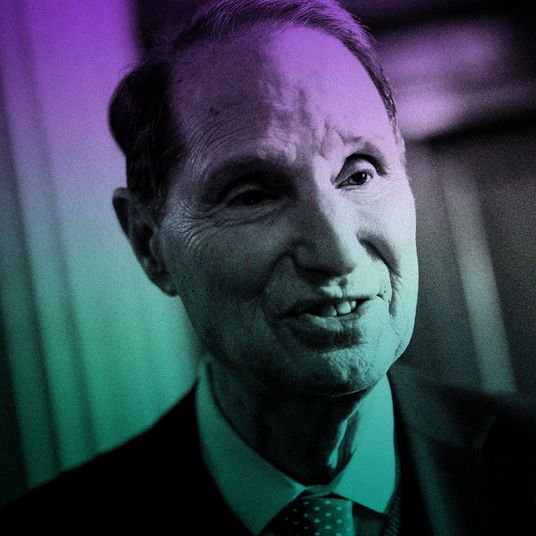
For much of the pandemic, Harvard epidemiologist Michael Mina has been just about the country’s biggest and most enthusiastic proponent of mass testing. For most of the year, the country has been relying on PCR testing, which is relatively expensive and typically returns results in (at best) a few days. In some places, there has also been rapid molecular testing, which works on the same basis as a PCR test — it looks for viral RNA, and can pick up even very small amounts, which means almost no one receives a false negative result. But for the last few months, Mina has been especially focused on the public-health potential of a different method, the rapid antigen test, which functionally measures infectiousness — rather than infection — and which is extremely cheap and easy to use. The closest analogy is an at-home pregnancy test — not quite as clinically reliable as a pregnancy test in a doctor’s office, but so much more affordable, available, and easy to access that it allows for a massive expansion of testing capacity. In mid-November, Mina argued that large-scale deployment could stop the spread of COVID-19 by Christmas — many months before even the most optimistic timeline of vaccine rollout could be completed.
What is the state of rapid testing right now? How many tests are being produced, and how many are being used?
Right now, in the U.S., we really are not using many rapid antigen tests at all.
What about elsewhere in the world?
Slovakia has had exceptional results. They rolled out exactly the kind of testing program I’ve been pushing, though not at-home testing. They asked half of their country to get tested over a weekend and then did that three weekends in a row. Within a few weeks, they saw incidents drop by like 50 percent.
It’s actually almost precisely 50 percent. They had a peak of 466 cases per million on November 4, and that dropped to 232 per million by November 24. Caseloads in other countries in Europe have been dropping, too, of course — often accompanied by lockdowns — but that Slovakia record is very impressive.
They had an increasing epidemic. It was exponentially increasing. And they just squashed it. Which makes sense. They found a lot of positives all at once and they stopped all of those positives from transmitting to others.
Now Austria will be rolling out a similar program. And Liverpool is rolling one out. Liverpool just had, from what I hear, very good success. They were able to drop incidents by something like a half or two-thirds over the first few weeks of their massive screening program. I believe Poland is about to roll this out as well. So we’re getting more and more evidence. And then we have lots of evidence from us.
What do you mean?
Every college in New England that’s doing frequent testing. You know, it doesn’t matter if it was PCR or antigen testing — it’s the frequency that really matters. What we’ve seen is that where there is frequent testing, outbreaks just aren’t happening.
And the cost of rapid antigen testing means, theoretically, you could do much more frequent and widespread testing with them. What’s the national capacity look like right now?
The government bought around 150 million of Abbot’s paper-strip tests, but they weren’t actually manufactured yet, so really they bought the production capacity. That’s about it. Access Bio is another rapid-test company that got an emergency-use authorization and we’re starting to see them be used more frequently. Whereas Abbott can build around a million a day given current capacity limits, Access Bio can build about 500,000. They’re a pretty small company; they’re ramping up to build between 2 and 3 million a day as we move into January, February, and March.
That’s 1.5 million being produced right now. You’d like to see 10 or 20 million per day, I think, right?
I think we could be seeing many, many more of them available if there was actually some agency in the government behind it, but that’s kind of where things are at.
Is that also roughly how many rapid tests are being used right now — about 1.5 million per day?
No. There’s a big stock of these Abbott tests that aren’t really being used.
Why not?
They’re controlled by the government, so they’re not on the market. The government bought them all, and they’re kind of, sort of being distributed, but not utilized, because nobody really knows how to use them. It’s not rocket science, but there’s just been no plan. And there’s so much confusion about, are they accurate?
How do you answer that question?
I mean, Abbot’s BinaxNow test is exceedingly accurate. It’s an extraordinarily accurate device. It’s very, very good for what its use is.
You’ve said that in detecting contagiousness they are more than 98 percent effective. And if you add a second, confirmatory test, it elevates the specificity of the test to greater than 99.9 percent.
But as recently as two weeks ago, there was a headline in the New York Times saying that these tests are inaccurate. It was just completely a wrong interpretation of the data.
How would you like us to interpret it?
The discourse should not be about accuracy — about whether or not rapid antigen tests are less accurate than PCR tests. Accuracy is entirely dependent on what your target is. And so, sure, if your target is PCR detection of RNA, then an antigen test just won’t work, because it literally doesn’t pick up RNA after the virus has gone. But if the target is infectious people — which is really the most important public-health target — then these tests become extremely accurate. And that’s the issue — we shouldn’t be using a medical target, we should be using a public-health target. If they are being used for medical diagnostic purposes, they might not be as accurate as you would like, but as a public-health tool, they’re very accurate.
Rather than asking, can using this test help us control the spread of the disease, we’re asking, is the result of this test reliable enough to serve as the basis of treatment. But holding all tests to that standard means the tests we do use will be less useful in controlling spread.
That’s why I’m so adamant that we have to stop thinking of this as a medical test. We need to have these be evaluated, considered, authorized, distributed all as public-health tests. And that means the metrics are different. It also means that we have to create different, simple sets of instructions, so people know how to use them. The real problem is we just have failed so miserably in this country to even consider it as a different kind of test than a medical test.
And what that means is that we need public-health authorities to step in and say, “Hey, you know, we’re sending a million tests to a bunch of people who know nothing about testing in nursing homes.” Maybe we have to do something that’s not business as usual. Maybe we have to actually tether two tests together and say for every 10 or 20 tests of this type, we send two confirmatory tests with very simple instructions. That alone would make all the difference. But to do that would demand that these institutions recognize that this is a public-health problem. And they have yet to recognize that the testing required for this public-health catastrophe is a public-health test. You know, they keep treating it as business-as-usual medical diagnostic tests, clinical tests.
And the media coverage is truly doing damage on this point. I mean Katherine Wu’s single New York Times article a couple of weeks ago led countries to stop using these tests. I don’t think the press is fully realizing how much power they wield when they write these articles in the middle of a pandemic. Because the press is as on top of the science as anybody
We’re often writing about preprints or other research that hasn’t even been published yet.
And so policy-makers are listening to the press as much as they are anyone else, and this is a unique position for media to be in. And I really think that it is a major problem.
This is a national emergency, this is a war that we’re in. And instead of putting generals in positions of power, we’ve deferred to academics by and large. And I actually think this is a major mistake because academics are not trained to make decisions with the best knowledge available at the time. They’re trained to make decisions based on Nature papers they read ten years ago. They’re not trained to adapt to the environment, to the ecosystem. They want academic precision, they want p-values and statistical significance. And that’s really different from a general in an army. They have to get comfortable like a surgeon does with working on imperfect information, and academics don’t do that. The fact that we’re still squabbling over antigen tests and trying to figure out, well, what if it doesn’t catch somebody with a CT value of, of 32, but it does somebody with 30 — we are completely missing the point in all of this! If a general was making decisions, they would say, “Is this the test that catches the most infectious people? Yes. Okay. Well then we’re doing it, we’re using it.” That’s the mind-set we should have had; instead we have this academic precision and it’s really screwing us up in terms of being able to act swiftly and with the sort of urgency that we need.
But technically, rapid antigen tests are less accurate if you’re applying a diagnostic standard. They are also potentially more appealing because both they focus on infectiousness and because they are cheaper and faster and could be deployed at a much larger scale.
Of course. And you really cannot — we cannot — under any circumstances start to deploy antigen tests without giving confirmatory antigen tests or some other rapid confirmatory tests right along with it. Because we know that these tests, especially the earlier versions, were giving false positives — maybe like one percent or a half a percent of the time. That’s like one in every 100 or one in every 200 tests. That can be really bad if you’re distributing these, for example, to a nursing home where people are going to potentially cohort positives with positives. You definitely don’t want to get a false positive in a nursing home and take that false-positive person who’s actually negative and put them with a bunch of positives. That is potentially a deadly mistake.
There are ways around this problem, but we have to use some strategy. The easiest way is what we always do in laboratory medicine or diagnostics and testing, which is if you have a screening test that has false positives, that’s sometimes desirable. You want to get the best screening test to find as many people as possible. And once somebody tests positive, you don’t call that a positive. At that point, you then run a confirmatory test, right? It’s not that the first one was falsely positive. It’s how the algorithm was supposed to work.
It’s how HIV testing has often been done: The rapid test is basically screening for potential positives, those potential positives would then take another test to be sure.
But early on, the government sent a bunch of molecular rapid tests to a lot of nursing homes. These are not antigen tests, but they’re still rapid and useful. And in Nevada, in particular, they found a number of false positives, but they didn’t have confirmatory tests, because the CDC had given them really no guidance. Except to say, if you get a positive, get a PCR test. But you can’t give somebody a five-minute test and then tell them to confirm it with a four-day test.
Four days can be optimistic sometimes.
I mean, it’s just completely insane. You just can’t do it. So we have to, if we’re going to deploy these and we want to keep people safe and keep public confidence in them we can’t have one percent false positives, and we can’t have all those people have to go way out of their way to get PCR tests or get cohorted inappropriately. So we have to do something different, and that wasn’t done and it still is not. It’s barely being discussed. I mean, I’ve been trying to push it as much as I can for months and months and months.
But no luck in making the case that the proper action there is a confirmatory test?
Frankly, the FDA — when I went to the FDA and the CDC they just kind of rolled their eyes at me. I mean, truly. They said, “Well, it’s not really a problem.” The FDA said, “That’s not how we evaluate these products. We do it one at a time. And if they want to be paired with a confirmatory test, great, but that’s not our issue.” It’s just another one of these things during this pandemic that was completely, completely predictable — completely foreseeable and preventable.
I’m curious, why do you think the FDA and the CDC have managed things so poorly? I mean, this is one example, but there’ve been a number of others where they’ve made what seemed at the time, to those who really understood the issues, to be quite destructive decisions.
This is a current thing — I’m still badgering them all the time to say, we have to build confirmatory tests that are rapid, and they still haven’t done it. But, yes, it’s the same problem that’s been going on throughout the pandemic. Like, why did the CDC screw up so badly in February with the PCR tests?
You mean insisting on developing their own test, rather than just allowing the one approved by the WHO to be used.
It didn’t make any sense to me then and it still doesn’t. I think part of it is that they are stretched thin. These agencies have been underfunded for a long time. But that’s not really an excuse.
What’s the problem, then?
I think it all stems from the top. There was probably immense pressure in February to get these tests out, and a worst-case scenario would be that it was a directive that, hey, the U.S. has to make its own thing. We can’t follow others.
But the issue of rapid testing and needing a rapid confirmatory test — this is quite easy even for me to understand. If you’re talking to regulators with expertise in this area, wouldn’t you expect they’d understand, too?
I think one of the big reasons is because we are still seeing this really frustrating approach to this pandemic, which is continuing to just treat this as business as usual. One of the problems with business as usual is that every test in America is treated as a medical test. Every single test is getting evaluated as that.
So how can we change that perspective?
Well, I think we need the media to start writing better headlines.
Oh, it’s on us?
No, I mean, not just that. I think that one very good thing would be the CDC making some statements, but it might be five months before the CDC or the FDA make a statement because they’ve been months behind on everything — even at the most simple things like masks, or is this a pandemic or is this airborne. It’s just been astounding.
If the government did get onboard, the next step would be scaling up, presumably.
Oh, absolutely. I mean, we definitely need to scale up production.
How hard would that be?
It’s pretty simple. This isn’t like trying to scale a PCR production or a scale of vaccine production. There is one small factory in Paramus, New Jersey, that makes 500,000 a day and is scaling up to 2 million per day. As a nation, we just need about 10 to 20 million per day. So if the government really wanted to do that, that is not hard to do at all. It sounds like a lot of tests to produce, but I think people are overestimating how difficult these particular tests are to produce. That’s the beauty of them. There’s companies in South Korea making tens of millions of these. I’ve talked to the leaders of a bunch of these companies, and they say, “Yeah, the hardest thing is finding the real estate.” That shouldn’t be an issue. Buy a warehouse, put a billion dollars towards it, and you’d have it done in a month.
A billion dollars sounds like a lot, but Operation Warp Speed cost $2 billion and a lot of people think that was a drop in the bucket.
If this was a trillion-dollar enterprise, then that would be a different question, but this is $500 million to $5 billion investment. That’s absolutely nothing. That’s the part that really is driving me insane. We’ve already spent $5 trillion on this virus — how many billions does that work out to each day? Five trillion is 5,000 billion, so that’s like billions and billions of dollars every single day that we’re spending on this virus.
People often have a hard time conceptualizing the difference between a billion and a trillion. Like we just think of it as like big numbers. But one is a thousand times bigger than the other.
Exactly. People think $5 billion is a lot, but $5 billion is literally like 12 hours of this virus right now. Why wouldn’t you do it? I mean, it’s just so hard to see people even bring up dollar signs as a barrier here. I mean, heck, you know, Mark Zuckerberg or any one of the wealthy people in this country — or get a bunch of millionaires together! — could invest a hundred million dollars into Access Bio today, not for prepayments, but just specifically for capacity building. If that happened, they could build a new factory in a month.
Do you think there’s any chance we see movement soon — in a new stimulus package, for instance? Or will we be waiting until January 20th and the new presidential administration for any of this to start happening?
I think we’re going to have to wait. I don’t really anticipate any bold steps being taken from this administration. What I would have liked to see months ago, many months ago, is the government recognizing that this is like a war that we’re fighting.
What would that mean?
Having the federal government not serve as a barrier to entry for these tests, with the FDA. I would’ve liked if the federal government stopped doing things as “business as usual,” where they just kind of say, “Well, we’ll accept your application and we’ll try to get it through our portals as quick as possible.” At this point, if the government actually wanted to do it and put their resources behind it to say, where there’s a will, there’s a way here. We’re going to give you troops to help you build the walls or whatever, you know, whatever it might be. I believe very firmly that it would not be a difficult thing to get a factory like this built in a month.
How would you distribute the tests?
Postal service.
Directly mailed to people’s homes?
Yeah, I think it’s the only way. I mean, heck, I won’t go a block out of my way to get a test right now. I never leave my house. The moment they’re not in the home, you’ll lose the ability to do frequent testing. People aren’t going to go to a site and stand in line — it’s dangerous because you have to stand in a line with other people.
So everything is self-administered?
These are like dead-simple tests to use. People say, well, what if people will do them wrong? But you can make the information so ubiquitous, get everyone involved — news anchors, celebrities. It’s like a wartime effort, and you just get everyone involved in communication and education. It’s a collective effort. And unfortunately, we keep treating this as though it’s some capitalistic effort — an every-man-for-himself kind of approach. That is not how you solve a public-health crisis.
But in a way, the system that you’re describing to me does sound like every man for himself, because you’re still depending on people basically surveilling themselves, testing themselves, and then responding to that information in a certain way — a responsible way, say by quarantining. To me, that’s another couple of layers of human complexity you have to account for. The modeling is totally persuasive to me — you have Americans taking tens of millions of tests per day, the numbers will go down. But how much depends on how we respond to that information, right?
Yeah, absolutely.
Other countries in the world — especially in East Asia — have had a kind of medical surveillance state that stood up in response to this pandemic. Not a total surveillance state, in most cases, but far beyond what we have here. What you’re proposing is basically that we ask people to take on the full burden and responsibility of that surveillance state themselves — to test themselves, and then to behave responsibly with the information they have, without anyone looking over their shoulder.
Yeah. But unless we’re going to lock them up, there’s no other way to do it. You’re either using a paternalistic top-down approach and you’re just telling them what to do, or you’re giving them the tools to do it on their own. And I think that one of the major differences between us and South Korea and China is that we live and breathe in this country in terms of individualism and freedom. The government’s not going to tell us at all what to do, is the mantra in the U.S. Masks and social distancing became political. But I’m convinced that most people in the country don’t want to get their friends or loved ones sick. This is an approach where people, I think, can be empowered to know their status, and maybe they still go to work, but maybe they don’t visit their mom. And maybe while they’re at work they keep their distance from their friends, don’t have lunch at the same table with them.
In some ways I think the individualism thing can be overstated — for a few months you had pretty strong compliance with shutdown orders, which were relatively draconian. And you mentioned masks and social distancing — there is a way of looking at that, that it was politicized and imperfect, and that’s obviously true, but it’s also the case that a lot of people are wearing masks and a lot of people are social distancing. I often think we have a tendency to see anything short of a perfect rollout as unacceptable when in a situation like the one we’re in now, partial victories are still victories. Getting to 70 percent compliance is better than zero percent compliance — with masks or rapid testing or anything else.
That’s exactly right. And I think that what we saw early on was the government saying, “Don’t use masks. They’re not perfect.” And of course, now we know that that’s ridiculous, but this is an age-old concern. Don’t use seat belts, they could cause people to drive more recklessly. Don’t use a pregnancy test, it could cause somebody to drink more if they’re negative. And on testing, as with masks, you’re absolutely right, there’s a lot of people who are willing to comply. There’s a lot of people who are begging to have these tests in their homes and available to them.
But even more than that, there’s something special and unique about these tests that could make them more palatable than masks and social distancing, even in those places where masks and social distancing have been politicized. Two things, really. One is, it requires very little energy. If it’s in your home, it requires 30 seconds of work — you know, you brushed your teeth and now you take a COVID test. It’s really that easy. Wearing a mask and distancing is a lot of energy. That’s a lot of energy expended every day to do that. But even more important, I think to a lot of the people in this country, a mask and social distancing are part of a social dynamic.
In some places it’s basically obligatory to wear a mask, and in other places, at least in certain communities, it’s almost the opposite.
But these tests are completely private. They’re empowering somebody, but doing it in private. You can have voluntary reporting. You can have the government do it, or with Google or AT&T — make it one-click reporting, but voluntary. I think that that’s important for a lot of people in this country too. You know, they don’t want to announce this stuff. They don’t want the government in their business. They don’t want all the surveillance stuff. They truly just want personal information. They want to keep it personal. And you know what? No wonder. We tell that to people every single freaking day — we say, “Your private health information is your private health information.” And these tests can be completely private. Nobody has to know. People can make whatever behavioral changes they want to make. So even the most hardened, non-mask-wearing guy, a guy in Wisconsin or Montana who, you know, doesn’t want his buddies to know that he is interested in this virus at all — he still doesn’t want to kill his mom. And he knows that he goes to work every day, and there’s a lot of COVID, and his mom’s 85 years old. Even somebody like that who might not be willing to wear a mask would be willing, I believe, to use the test in the privacy of their own home. It takes 30 seconds to do and five, ten minutes later, they see a line or they don’t. And they see the line and take a confirmatory test. Then maybe they just call their mom and say, “Hey, mom, I’m not going to make it tonight.”
So how quickly could this all happen? We talked earlier about it not even beginning before Joe Biden is sworn in. From there, you say, production could be scaled up in about a month. That brings us to March 1, and I wonder how you see that playing out alongside the timeline of vaccine rollout. Obviously if we had done this six or nine months ago, we would be in a much, much better shape, but how much of a difference would it make it a world where tens of millions, or perhaps even a hundred million, Americans have been vaccinated by spring?
Well, I think late spring would be a way overestimate for when most people in America will get a vaccine. You know, it requires a lot to produce and deploy vaccines. The vaccines are going to come, yes.
But, frankly, we’ve been talking about the vaccines that way since May, like they’re just around the corner. Now, whether it’s been as overt or not, people have acted with a lack of urgency because the vaccine has always been one month away, one month away, one month away. Of course it hasn’t actually been a month away. And even now, it’s still one month away. When in reality, it’s probably gonna be like June. And even then we don’t want to put all our eggs in the vaccine basket.
Why not?
We don’t know at all how well it’s actually going to do four months after somebody gets a vaccine. We haven’t actually measured that. And there’s really good reason to be extremely concerned about that. The vaccine efficacy, so far, is wonderful — 90 percent, 94 percent efficacy. But that’s because we’ve only so far evaluated it for a few months. Those results are probably going to fall rapidly after three months.
Wait, what?
You know, I haven’t heard a lot of people talk about this yet, unfortunately, but it needs to be taken really seriously. There’s a reason we don’t normally measure the efficacy of a vaccine within a two-month window. And that’s because when you get a vaccine, your body elicits an amazing immune response. It doesn’t matter what the vaccine is — even crappy vaccines will elicit a really strong, robust, what we call plasmablast response. And that’s just part of your inflammatory system’s response to an infection — to clear it, you want to sort of create a huge number of cells that produce antibodies, right?
But the important thing to recognize is that those cells that your body creates— it makes billions and billions of these, and yet by definition, 100 percent of them die off after two or three months. And this is because they are literally temporary cells. They’re just there to respond to the invader, and you’ll go from having like 20 percent of all of your cells in your blood that are this kind of cell, to almost zero four months later. And we have only measured the efficacy of these vaccines during the window of time when these cells persist, right? So of course, you’re going to have these amazing efficacy results.
That doesn’t sound very encouraging.
It does suggest that the target that we went for is the right one, because the cells are working to clear the virus. But let’s go back to the war analogy. This is akin to sending 100,000 troops to the front line, and they successfully hold off the enemy. But what happens when you completely remove all of those troops and you replace them with just a few snipers in towers? Maybe the snipers will hold off the enemy, but there’s no good reason to necessarily think that the snipers will hold the line nearly as well as when you’re at 100,000 — or in this case, a billion troops right there at the front line that all disappear.
I’m hoping that we will see a continued robust response, but we don’t actually have good data. So I think we just have to take these early efficacy results and remember they are early results. We shouldn’t be putting all of our plans for other approaches on hold because of a 94 percent efficacy when we don’t even know, is this efficacy going to hold just for five months?
What do you think? If we’re now, at this juncture, seeing efficacy somewhere roughly in the 90 percent range, what is the range you think is possible five months from now, or a year? How low could it get?
I think the range could go anywhere from staying where it is to falling to about 50 percent. You know, it could be that these neutralizing antibodies are really potent and that you just need a few long-term, long-lived memory cells that migrate into the bone marrow. That’s where the sniper-in-the-tower metaphor comes from — those sniper cells are called long-lived plasma cells or memory cells. And they go to the bone marrow. And so if they’re producing enough antibody to really neutralize the virus, and they turn out to produce really, really potent neutralizing antibodies, well, that might be good enough. You know, maybe we will see a continued 90 percent. But my guess is that it won’t stay at 90 percent if we actually do go and measure people from like four months to nine months from now. Maybe we’ll see efficacy fall down into like 80 percent, but there’s a chance that it could fall to like 50 percent. And that’s what we don’t know. We just don’t know how big that range is really going to be.
And that all means the vaccine might not stop transmission as much as we think. On top of that, the important pieces the virus could mutate at any time. We don’t know how long it’s going to take this virus to escape immunity. But we do know that we have effectively created one vaccine — all of these vaccines are identical. The mode of administration is different. The vector, whether it’s some RNA or an unknown virus, is different. But they all express the exact same protein. And we have never gone through a global ecological experiment like the one we’re about to go through — a global pandemic forced through a single bottleneck.
We are putting so much ecological pressure on this one virus with these vaccines. And all it takes is one virus out of the quadrillions of viruses that are being produced across the globe right now in people’s bodies — all it takes is for one of those viruses to say, you know what? I want to figure out how to evade this person’s immune response. And if we have a whole population, a whole human population that has been vaccinated with one protein … It’s astounding to me that this isn’t, like, considered a crisis.
Now, I believe very firmly that these vaccines will work, but I am extremely cautious about being so flagrant in assuming that there’s no chance that mutation is going to happen. Given the gravity of this situation, why the heck are we not making contingency plans for new vaccines as well?
And you think rapid tests can be our contingency plan, too.
These tests can be our backup. If we get people socialized to using these tests, we don’t have to find ourselves in this position again. And you know, what if another coronavirus pandemic comes around in three years, or the flu, we can use these tests for that too. The tests can be adapted to any of these viruses. So it’s also part of a global preparedness plan for future pandemics.